1. Introduction: Brief on Elinor Ostrom’s Work & Why It Matters for Drug Coverage
In the preceding articles of this series, we’ve investigated how the conventional, centralized drug coverage model struggles with transparency, fair pricing, and patient access. We’ve introduced the concept of enumerating coverage nodes, explored ways to build exhaustive parameter libraries, and discussed potential open-access infrastructures and pilot projects that might redefine how stakeholders manage benefits.
Now, we look to Elinor Ostrom, the first woman to ever win the Nobel Prize in Economic Sciences, for guidance. Ostrom’s work focused on how communities govern shared resources—like forests, fisheries, and irrigation systems—without succumbing to the “tragedy of the commons.” Her perspective, encapsulated in her Institutional Analysis and Development (IAD) framework, provides a powerful lens for understanding how multiple stakeholders can collaborate effectively. Though Ostrom’s research originally revolved around natural resources, the same principles of polycentric governance and institutional diversity can be applied to healthcare—especially the realm of drug coverage.
In this article, we’ll break down Ostrom’s core ideas and show how enumerating drug coverage nodes within a more institutionally diverse ecosystem can mitigate power imbalances, encourage robust stakeholder participation, and deliver more equitable, cost-effective care.
2. Positions, Rules, and Action Arena: Breaking Down Key Elements
Ostrom’s Institutional Analysis and Development (IAD) Framework
The IAD framework is a conceptual tool used to unpack the complex interactions between individuals, organizations, and rules within any “action arena.” According to Ostrom, three foundational components drive outcomes:
- Positions – The roles or identities that participants can assume. For drug coverage, these might include:
- Pharmacy Benefit Managers (OptumRx, CVS Caremark and Express Scripts)
- Plan Sponsors (employers, governments, or coalitions/consortia)
- Manufacturers (pharmaceutical companies, biotech firms)
- Patients (individual beneficiaries, advocacy groups)
- Pharmacists and Clinicians (practitioners making everyday decisions on medication therapy)
- Payers/Insurers (traditional insurance plans, third-party administrators)
- Rules – The formal and informal constraints that guide actions within the system. In a traditional drug coverage context, rules might include:
- Contractual agreements over drug pricing or rebates
- Regulatory requirements (HIPAA, state mandates, etc.)
- formulary management protocols (e.g., prior authorizations, step therapy, quantity limits)
- Informal norms (e.g., how PBMs negotiate behind closed doors)
- Action Arena – The “space” (physical, digital, or both) where stakeholders interact, negotiate, and ultimately make coverage decisions. Within drug coverage, this could be:
- Boardrooms or online meetings for P&T (Pharmacy & Therapeutics) committees
- Industry conferences and presentations
- Virtual infrastructure for claims and request processing
- Regulatory hearings that shape public policy
- Physical and online pharmacies and wholesalers
By outlining positions, rules, and the collective action arena, Ostrom underscores that governance isn’t limited to top-down directives. Instead, the participants who occupy various positions can enact and reshape rules to produce outcomes that align with shared goals—in our case, equitable, cost-effective, and transparent drug coverage.
3. Institutional Diversity Meets Drug Coverage: Examples of Node-Based Ecosystems
Why Polycentric Governance Matters
Ostrom’s concept of polycentric governance posits that multiple centers of decision-making—each with some autonomy—can lead to better collective outcomes than a single, monolithic authority. In a drug coverage system dominated by a few large PBMs, we often see power imbalances and opacities in pricing, utilization management, and negotiated rebates. Enumerating coverage nodes and distributing decision-making more evenly can:
- Foster Competition – Multiple coverage nodes allow different coverage models to compete on pricing, quality, guideline integration or clinical appropriateness.
- Empower Local Knowledge – Employers and patient groups can tailor coverage criteria to local needs (chronic conditions prevalent in a given population, for example).
- Reduce Exploitation – When more decision-makers share power, it’s harder for any single entity to exploit information asymmetries or enforce inflated costs.
Example: A Multi-Stakeholder Action Arena
Imagine a node-based ecosystem with various specialized consortia:
- Employer Consortium Node
- Self-insured employers collaborate to create a formulary reflective of workforce demographics.
- Local knowledge drives coverage decisions (e.g., higher coverage of diabetes treatments if local data shows a surge in Type 2 diabetes).
- Rare Disease Node
- A coalition of manufacturers, clinicians, and advocacy groups set rules for cost-sharing on high-priced therapies. Value-based agreements are still in their nascent form and could potentially rise in utility with more transparency and access.
- Each participant has a defined position (manufacturer offering price concessions, patient groups advocating for coverage, etc.), formalized through enumerated coverage criteria and their associated price.
- Incorporating Independents
- Local pharmacists, smaller payers, and patient representatives form a “coverage node” to address community-specific challenges (e.g., rural pharmacy access).
- They negotiate direct deals with manufacturers for essential medications, documented in an open platform, ensuring transparency and accountability.
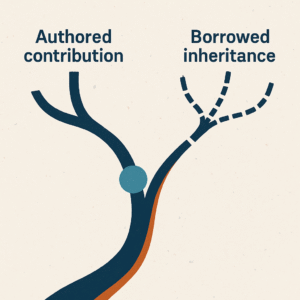
By distributing coverage decisions across several “centers” of governance, the ecosystem more closely resembles Ostrom’s polycentric ideals—where each node experiments with coverage strategies, shares insights, and collectively drives improvements in price and access. I dub this activity as play restoration within the pharmacy benefit space.
4. Benefits & Challenges: Ensuring Accountability, Avoiding Overly Complex Rule Systems
Benefits of an Ostrom-Inspired Model
- Greater Stakeholder Buy-In
- When stakeholders see they have a legitimate seat at the table—and the ability to co-create or amend rules—they’re more likely to align with outcomes and propose innovative solutions.
- Custom-Tailored Solutions
- Decentralized nodes that use local population data can refine node configurations to meet real needs—improving patient outcomes and potentially reducing wasteful spending on ill-fitting or poorly negotiated therapies. This is also valuable channel feedback for manufacturers that might not get granular claims data insights.
- Checks and Balances
- Multiple decision-making hubs mean power is diffuse; no single entity can dominate or manipulate coverage rules to maximize short-term gain.
Potential Pitfalls and Complexity
- Risk of Fragmentation
- Too many autonomous nodes may lead to inconsistent coverage decisions or confusion for patients who move between regions or change employers.
- Overly Complex Rule Systems
- Enumerating every single coverage criterion across multiple nodes risks drowning the process in bureaucracy. Ideally, this will be done in a manner that facilitates more competition without adding administrative burden.
- Technology platforms must be robust enough to handle these complexities without overwhelming users (see Part 4 for open infrastructure recommendations).
- Coordination Overhead
- More centers of governance can mean additional layers of coordination. Disputes between nodes (e.g., coverage overlaps or cost-shifting) must be resolved efficiently to maintain system integrity.
5. Practical Application of Ostrom’s Principles
Local Knowledge and Adaptability
Drawing on Ostrom’s emphasis on local knowledge, each enumerated drug coverage model can be tailored to a particular population’s demographics, disease prevalence, and fiscal constraints. This flexibility allows for “experiments” in coverage to see which rules produce the best outcomes for specific communities, conditions, or drug classes.
Translating the “Tragedy of the Commons”
In the context of drug coverage, the “commons” can be seen as the pool of healthcare resources (drug budgets, shared risk pools, or public funding). If a coverage system is skewed toward high-cost medications without oversight, resources may be depleted—or allocated inefficiently—harming patients who rely on sustainable access to necessary drugs. Enumerated nodes introduce checks and balances similar to existing coverage management strategies with the added bonus of making coverage rules transparent and distributing additional decision-making amongst informed stakeholders.
Conflict Resolution Mechanisms
Ostrom’s framework highlights the need for conflict-resolution mechanisms, which might include:
- Independent Mediation – A neutral third-party reviewing coverage disagreements on pricing or meeting node conditions.
- On-Chain Governance – For those interested in blockchain approaches, smart contracts could automate decision logic and handle disputes based on preset rules.
- Consensus-Building Platforms – Online forums or regular consortia meetings where stakeholders propose changes, debate coverage strategies, and vote on updates.
6. Conclusion: The Value of Ostrom’s Insights in Decentralizing Healthcare
Elinor Ostrom’s legacy demonstrates how diverse groups, armed with the right rules and frameworks, can govern shared resources more effectively than systems controlled by vertically integrated authorities. Applied to drug coverage, Ostrom’s IAD framework illuminates why distributing decision-making among an expansive network of coverage nodes can:
- Unlock Local Innovation – Encouraging smaller groups to tackle coverage problems head-on.
- Reduce Monopolistic Power – Mitigating the outsized influence of a few large PBMs or payers.
- Enhance Transparency – Clarifying pricing and coverage arrangements for every participant in the action arena.
As we push toward more polycentric governance in healthcare, the lessons from Parts 1–5 of this series—building exhaustive parameter libraries, exploring open-access infrastructures, negotiating conditional pricing—gain a deeper ideological grounding through Ostrom’s research. Her scholarship reassures us that institutional diversity is not only possible but often preferable, preventing exploitation and fostering more equitable resource distribution.
In charting the future of drug coverage, we have an opportunity to replicate Ostrom’s success by designing systems that treat medication access as a shared resource. Through clearly enumerated coverage nodes, transparent rules, and a multiplicity of action arenas, we can chip away at entrenched power structures and arrive at a more just, patient-centered model of healthcare. The next step is to continue refining governance models, conflict resolution mechanisms, and local data-driven solutions—turning a once-impenetrable insurance ecosystem into a vibrant community of stakeholder collaboration.