1. Introduction: Why a Gradual Approach Is Essential in Healthcare
Over the past six parts of this series, we’ve charted a path away from the traditional, centralized drug coverage model—where pharmacy benefit managers (PBMs) often operate with opaque contracts and negotiate on behalf of payers—and toward a system that fosters enumerated node-based coverage and greater stakeholder collaboration. From tracing the origins of drug coverage centralization in Part 1 to exploring Elinor Ostrom’s polycentric governance in Part 6, each article has built a case for transparency, accountability, and flexibility in managing pharmacy benefits.
However, large-scale transformation in healthcare rarely happens overnight. Gradual governance transfer, where traditional PBMs are phased out in favor of distributed, multi-stakeholder models, allows for a smoother shift with fewer disruptions in patient care. As Vitalik Buterin suggests in his essay on encapsulated complexity, legacy systems often bundle and “prettify” risk in ways that ultimately obscure the true costs and constraints. Simply blowing up these structures—without a transition plan—risks chaos. Meanwhile, drawing on Frédéric Bastiat’s advocacy for free exchange and minimal barriers to trade, we see an opportunity to unbundle these middle layers, reduce overhead, and encourage direct negotiation between manufacturers, payers, and other stakeholders.
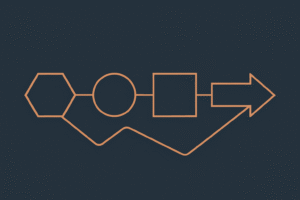
This seventh installment outlines a three-stage process for shifting governance from centralized PBMs to a more diverse, node-based architecture, while preserving continuity of care. We’ll also propose realistic timelines and milestones, recognizing that each step requires deliberate experimentation and coalition-building—rather than abrupt upheaval.
2. Defining Governance Transfer: Key Concepts (Control, Accountability, Transparency)
Control
In a centralized PBM model, control is concentrated in the hands of a few intermediaries. PBM professionals negotiate prices, build formularies, and determine rebate structures with variable degrees of oversight from employer groups, patients, health systems or clinicians. In a distributed model, control becomes more horizontal—with multiple stakeholders co-creating and negotiating coverage criteria nodes, sharing risk, and participating in consensus-based decisions. Over time, each stakeholder (e.g., self-insured employers, manufacturers, pharmacy networks) gains more direct agency over coverage terms and cost-sharing arrangements, which should lend to a more vibrant market, especially for smaller pharma players.
Accountability
Decentralizing control means rethinking who answers to whom. In an enumerated coverage node framework, transparency is baked into the process. This “open book” approach fosters accountability because every participant can see, and potentially challenge, the logic behind a coverage decision. Maintaining robust audit trails and establishing conflict-resolution mechanisms (as referenced in Part 6) become essential to ensuring the system doesn’t devolve into chaos.
Transparency
With encapsulated complexity, each layer of the existing PBM structure takes on risk or contractual obligations and then packages them in a “simplified” manner to the next entity—employers, insurers, or patients. This often hides real cost drivers and leads to confusion about who’s really paying. Ultimately, through premiums or through POS pricing, it’s likely the consumer (even consumers underutilizing their benefits!) Transparency means piercing these layers, making cost and coverage criteria plain. As Bastiat’s economic theories suggest, free exchange and direct negotiation only thrive when all parties have access to relevant information.
3. Three Stages of Decentralization: From Hybrid to Fully Distributed
Below is a phased roadmap for governance transfer, acknowledging that not all organizations will progress at the same pace.
Stage 1: The Hybrid Model
- PBM Coexistence
Traditional PBMs remain the primary coverage administrators, but some coverage nodes (e.g., high-cost specialty drugs) are carved out. For instance, a group of self-insured employers might create a direct contract with a manufacturer for certain oncology or inflammatory conditions products, enumerating coverage details in an open-access infrastructure (Part 4). - Minimal Disruption
Most existing contracts and claims adjudication pipelines stay intact. This approach reduces friction in the short term and provides a testing ground for enumerated node-based coverage, measuring its success on a small scale without overhauling the entire system. - Proof of Concept
During this stage, early adopters track metrics like cost savings, patient satisfaction, and operational efficiency. Benchmarking is important here, as the new product should bake in the “versus existing” efficiencies. This data helps build trust among more conservative stakeholders, showing that enumerated coverage nodes can reduce overhead costs and improve transparency.
Stage 2: More Payer and Manufacturer Direct Negotiations
- Expanding Node Coverage
As the initial pilots prove successful, the next wave of coverage nodes extends to a broader range of therapies or benefit classes. Competitive classes are relatively simple to define, with the help of Wolters Kluwers Medi-Span GPI coding system, leveraging categorical conventions from FirstDataBank, the FDA or even building novel frameworks to classify economically pertinent drugs. Employers who once depended entirely on PBMs now conduct direct negotiations with manufacturers for routine medications as well. - Transition of Control
The PBM’s role shrinks to managing narrower tasks—like claims processing—while price-setting and formulary decisions shift toward collaborative consortia or self-insured employer networks. - Tooling and Infrastructure
Platforms built to manage enumerated coverage nodes must be robust enough to handle a higher volume of transactions. Smart contracts, advanced data analytics, or simply well-structured cloud databases can automate key steps, from eligibility checks, to pricing, or new negotiation inquiries.
Stage 3: Fully Distributed Network of Node Operators
- PBM Obsolescence or Niche Role
Over time, PBMs might evolve into specialized service providers focused on technology, patient engagement or consultative roles, rather than broad gatekeepers for all coverage decisions. Meanwhile, self-insured employers, pharmacy networks, and “tech-savvy providers” operate their own nodes. - Multiple Governance Models
Drawing on Part 6’s discussion of Elinor Ostrom, communities can experiment with DAO-like structures (blockchain-based) or consortium-based oversight committees. Stakeholders may hold “tokens” or membership shares, with voting rights proportional to their role. As always, governance transfer should be taken very seriously to preserve community resources. The clinical component of decision-making will also need to be protected. - Market-Driven, Yet Collaborative
The final picture is a polycentric ecosystem where no single entity can dominate coverage negotiations. Employers, manufacturers, patients, and other node operators exchange information and services under transparent rules, aligning incentives for cost containment and better clinical outcomes.
4. Realistic Timelines & Milestones
12–18 Months
- Stage 1 Deployments: Small pilot programs carve out specific drug classes from PBM control.
- Metrics Gathering: Early data on cost savings, operational feasibility, patient satisfaction, and administrative burden is shared within participating consortia.
2–3 Years
- Scaling to Stage 2: As success stories accumulate, more employers and manufacturers adopt direct negotiations for a wider swath of drug benefits.
- Platform Maturity: Node-based coverage software or cloud databases reach new levels of reliability and user-friendliness, encouraging broader adoption.
3–5 Years
- Widespread Decentralization: Multiple stakeholders begin relying on node-based frameworks for the majority of their prescription coverage needs.
- Emergent Governance Structures: DAOs, co-ops, or alliances of employers, providers, and manufacturers form stable networks with built-in conflict-resolution and transparent revenue models.
5–7 Years
- Stage 3 Dominance: Fully distributed ecosystems become the norm in innovative pockets of the healthcare industry. PBMs, if they still exist, either specialize in consultative niches or transition into technology service roles.
5. Conclusion: Navigating Transition Without Disruption to Patient Care
Undeniably, a gradual governance transfer from centralized PBMs to decentralized, multi-stakeholder ecosystems is more than a theoretical exercise. It’s a tangible blueprint for addressing rampant opacity, inflated costs, and outdated coverage processes. As we’ve learned from Vitalik Buterin’s concept of encapsulated complexity, attempting to tear down old structures too quickly can backfire, introducing chaos in a sector where patient lives are literally on the line. Similarly, Bastiat’s belief in free trade reminds us that intermediaries shouldn’t obstruct direct exchange if both sides can benefit from more open negotiation.
By adopting a multi-stage roadmap, stakeholders can tackle the steep learning curve in digestible increments. Stage 1 lets organizations test coverage nodes in discrete areas without risking total system upheaval. Stage 2 expands on early successes by forging direct payer-manufacturer relationships for mainstream therapies. Stage 3 envisions a fully distributed environment—one in which node operators (employers, pharmacy networks, and tech-savvy providers) anchor a transparent, patient-centric coverage model.
All along, the focus remains on ensuring patients do not experience lapses in medication access or coverage clarity. Timely education for patients and clinicians, robust technology platforms for exhaustive enumerated coverage, and transparent communication across stakeholders are critical. For instance, updating internal workflows, reassigning staff to more strategic roles, and gradually retraining claims processors to support the new system can maintain stable operations.
Ultimately, this transformation resonates with the central themes of the entire series: an enumerated, patient-driven, and economically optimized approach to drug coverage. By addressing control, accountability, and transparency head-on, we pave the way for a future where coverage is not an impenetrable black box but a collaboratively shaped, data-informed continuum of care. In the upcoming final installment, we’ll examine how these changes position us to influence the P&T action arena and, ultimately, bring in a new era of drug coverage management.