Quick Answer
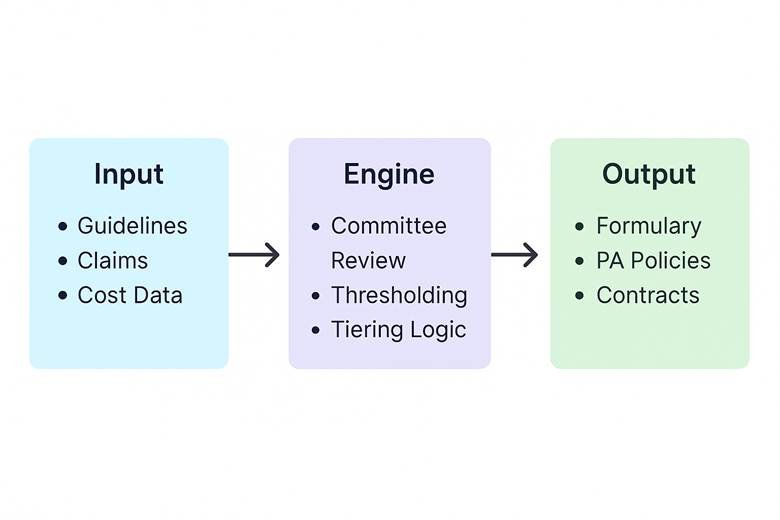
A value-based formulary is a structured approach to drug coverage that prioritizes clinical outcomes and cost-effectiveness over brand contracts or traditional rebate incentives. By tying coverage to value—defined as the therapeutic benefit per dollar spent—these formularies aim to improve patient care while ensuring financial sustainability for health plans and sponsors.
What Is a Value-Based Formulary (VBF)?
I think this is becoming more and more baked in to formulary setups today. Rebate chasing is still a part of the game, but plan sponsors are generally incentivized to drives cost down, so the best formularies, by definition, should incorporate value as the primary ingredient. Real-world evidence, cost-effectiveness metrics, and therapeutic outcomes are all a part of the coverage equation.
At its core, a VBF asks: Which medications deliver the best clinical results per unit of cost? Bang for your buck without sacrificing meaningful clinical integrity. It’s an active shift from reactive cost containment to proactive care optimization.
Example:
For inflammatory conditions products, a VBF might prioritize coverage for drugs with similar efficacy and a slightly more risk-on safety profile. Is saving $5,000 a month worth the 3% additional relative risk of getting a bad headache? These are tough, ethically charged trade-offs, and often bureaucratic because the decision-makers aren’t adversely affected either way. High integrity is required to truly consider the weight of the decision.
Why It Matters Now
-
- Escalating drug costs: Especially in oncology, rare disease, and chronic specialty categories.
-
- Payer pressure: Employers, Medicaid plans, and exchanges want transparent logic.
-
- Clinical sophistication: We now have outcomes data, claims analytics, and patient-reported outcomes to guide smarter decisions, and the precision compounds over time.
A VBF signals intentional stewardship of both money and medicine.
The 10 Steps to Designing a Value-Based Formulary
1. Clarify Your Objectives
Start by defining what success looks like. What’s the population adherence rate for drugs that positively impact chronic disease? How can we immediately achieve cost savings? Improved outcomes in a specific therapeutic area? Reduction in ER visits? Your immediate and long-term goal drives the rest of the strategy.
2. Assemble a Multidisciplinary Committee
Go beyond a typical P&T Committee. Include pharmacists, actuaries, clinicians, analytics MD specialists, nurses, business professionals, and a patient advocate. Diversity is multi-dimensional.
3. Review Clinical Guidelines + Real-World Data
Use FDA labeling language, current clinical practice guidelines (ADA, NCCN, GOLD, etc.) and supplement with actual claims, EMR data, pharma liaison research and outcomes studies. The more grounded your criteria, the better your downstream defensibility when an employer group contests your approach.
4. Establish Cost-Effectiveness Thresholds
I’m not the biggest fan of ICER, but incorporating generalized frameworks like ICER, QALYs, and budget impact models can help. Explicit thresholds help maintain consistency when comparing new entrants. What is most valuable is relatively thresholds. You must critically assess and compare like products.
5. Segment by Condition & Drug Class
Not all drug classes need the same intensity of review. Prioritize high-cost, high-variation categories: GLP-1s, biologics, 3rd and 4th line oral oncology meds, gene therapies, variably dosed drugs. Utilization rates might also drive the workload and attention for CM teams.
6. Design Outcome-Linked Tiering or Contracting
This could mean:
-
- Rebates tied to explicit objective treatment success measures (e.g., weight loss, viral suppression, cognitive decline rate, progression-free survival, severe bleed events)
-
- Incentives for generic use rates, or preferred product strategies
7. Implement Sensible Step Therapy & Prior Auth
PA and step therapy are key levers to support your VBF. There is beauty in well-designed coverage logic. As we know it, the nature of healthcare is that there are limited resources available, and the rules and criteria are built to consider this. At their simplest, use them to nudge patients toward proven first-line therapies. At their most complex, use them to offer ease of access to edge case patients by considering the exact coverage scenario required to meet coverage with clinically viable guideline support.
8. Build Real-Time Monitoring Infrastructure
You’ll need dashboards, claims scrubbing, and feedback loops to ensure the VBF is delivering. Get your models cooking, and view outlooks scenarios. Regular audits prevent drift and uncover your blind spots.
9. Pilot Before Broad Rollout
Start with one therapeutic class. Monitor access issues, appeals, and financial impact. Get feedback from prescribers and pharmacists, and in some cases, patients.
10. Iterate Quarterly, or Monthly to Achieve Excellence
A static formulary is a dead formulary. Revisit drug classes monthly, quarterly or semi-annually. Update based on new studies, pricing shifts, or internal outcomes data.
Common Pitfalls to Avoid
-
- Overweighting cost alone: A cheaper drug that doesn’t work isn’t value—it’s waste.
-
- Neglecting patient behavior: Value isn’t just efficacy—it’s adherence, tolerability, and access.
-
- Skipping documentation: Without rationale documentation, your decisions won’t hold up in audits or appeals.
-
- Failing to test assumptions: Your PA rules may seem solid on paper—but break when applied to real-world patient coverage scenarios.
-
- Lacking dynamism: The best teams are continuously improving and making incremental, accretive efficiency gains
Final Takeaway
A value-based formulary isn’t just a list of drugs—it’s a clinical, ethical, and financial instrument. My definition is captured in the Pharmacist Write formulary management white paper. When designed right, a formulary preserves trust among clinicians, plan sponsors, and patients alike. And while the upfront lift can be heavy, the long-term dividends—in better care and smarter spend—make the effort more than worth it.
If you’re building or refining your own formulary strategy, start here. Or better yet, co-create the future by sharing your lessons learned.