Why this matters
Coverage rarely changes overnight. It evolves through a predictable, stepwise sequence—surveillance, review, drafting, coding, testing, and release. If you trace the trail those activities leave behind (who did what, when, based on which source), you can explain denials, anticipate shifts, shorten appeals and see which initiatives save employers money. Below is a platform-agnostic walkthrough of how payers update policy, and how to build a clean provenance record at each step.
The lifecycle at a glance
- Market surveillance → P&T agenda
- Policy drafting & versioning
- Evidence packets for contentious calls
- Operational codification (PA logic, edits)
- SME testing & sign-off
- Production release & communication
Each stage produces artifacts you can capture and link, forming an auditable chain from source document to point-of-sale behavior.
1) Market surveillance → P&T agenda
What happens. Clinical and pharmacy teams continuously scan FDA label actions, safety communications, guideline updates, outcomes publications, competitor moves, and manufacturer positioning (rebates, outcomes guarantees, indication expansions). Candidates for change are prioritized and placed on a P&T agenda with a proposed disposition (maintain, tighten, expand, carve-out).
Provenance to capture.
- Source details: title, publisher, source URL, date collected
- Snapshot of each source (PDF or HTML capture)
- A simple hash of the file/text for integrity checks
- P&T agenda metadata: meeting date, agenda ID, presenter
Common pitfalls. Verbal updates with no link; unlabeled PDFs that change quietly; agenda items without a traceable source.
Move to make. Maintain a surveillance register—a living table that logs every trigger with link, snapshot, and hash.
2) Policy drafting & versioning
What happens. A formulary/policy pharmacist updates the policy or “program summary”: step-therapy sequence, covered indications, approval durations, and exclusions. Drafts move through internal review before they go to P&T.
Provenance to capture.
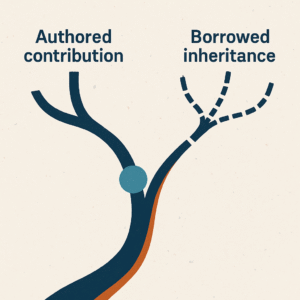
- Full criteria text block (verbatim), stored alongside a normalized summary
- Document version, effective date, line of business
- Author/editor and change note (“added renewal requirement…”, “updated step list…”)
- A criteria-block hash so you can prove when language actually changed
Common pitfalls. Headings change but criteria don’t; or criteria change without a new version.
Move to make. Treat the criteria like code—version it, keep the full text, and log a one-line rationale per change.
3) Evidence packets for contentious calls
What happens. When the decision isn’t obvious, reviewers assemble a mini-dossier: pivotal trials, comparative effectiveness, safety signals, real-world data, and any cost/value notes. The packet frames the decision for P&T.
Provenance to capture.
- Minimal evidence chain (trial → population → outcome → effect size)
- A confidence/grade tag (your internal rubric)
- Links/snapshots for each citation; reviewer notes
Common pitfalls. Copy-pasted PDFs with missing pages; “data on file” without access; no clarity on which endpoint moved the committee.
Move to make. Use a one-page evidence abstract template so every packet looks the same and cites the same minimums.
4) Operational codification (PA logic, edits)
What happens. Once approved, analysts translate policy text into logic that adjudicates claims: prior auth questions, step-therapy rules, edits for age/quantity, site-of-care, and exception handling. This is where ambiguous sentences must become yes/no checks.
Provenance to capture.
- The mapping from each policy clause → a concrete rule (e.g., “Initial Approval” → PA question set)
- Test scenarios (happy path, edge cases, denial cases)
- A cross-reference table from criteria lines → rule IDs in the adjudication system
Common pitfalls. Text says “preferred product” but rules don’t enforce it; renewal logic lost; differences by LOB not captured.
Move to make. Maintain a traceability matrix that shows, line by line, how text became rules and what each rule does.
5) SME testing & sign-off
What happens. Subject-matter experts validate that the rule implementation matches intent. Depending on workflow, this can be UAT in a sandbox or targeted prospective audits.
Provenance to capture.
- Named approvers, date/time, environment tested
- Test results (pass/fail), screenshots of adjudication outcomes
- Documented exceptions or acceptable deviations
Common pitfalls. “Looks right to me” emails with no test data; only positive cases tested.
Move to make. Require at least one negative and one borderline case per rule set; attach results to the change record. You can never anticipate all edge cases, but attempting to envision them is a huge value pickup.
6) Production release & communication
What happens. Rules are promoted to production. Provider portals, PA platforms, and pharmacy point-of-sale begin reflecting the new criteria. Member/provider communications and web policy pages are updated.
Provenance to capture.
- Release ticket ID, production timestamp, environments/promotions
- Links to updated public pages and PDFs; hashes of those files
- Who was notified (providers, brokers, internal teams), and how
Common pitfalls. Code updated before the public policy PDF; communications lag behind the effective date; rollback without documentation.
Move to make. Tie the release ticket to the public artifact and require a “public parity check” before closure. Uniformity in all channels can save you from high-risk conversations at inconvenient times.
A lightweight provenance checklist (platform-agnostic)
- Snapshot everything: store the original source files and policy PDFs that justify the change.
- Stamp every artifact: collected_at, effective_date, version, line_of_business.
- Hash key text: file, policy text block, and final criteria—so “what changed” is provable.
- Write tiny change notes: one sentence per change with the reason (“new indication approval,” “added step 1: X”).
- Map text → rules: maintain a human-readable table that links criteria lines to rule IDs and PA questions.
- Test visibly: keep pass/fail outputs and screenshots, including at least one denial case.
- Close the loop: link the release ticket to the public artifact (PDF/URL) and the communication sent.
What counts as a “material change” (quick triage)
When comparing versions, elevate these differences first:
- Step-therapy list: additions, removals, re-ordering
- Approval duration: initial vs. renewal, new response thresholds
- Indication scope: added/removed diagnosis or population
- Exclusions & safety: contraindications, required monitoring
- LOB divergence: Commercial vs. Exchange vs. Medicare language
- Soft wording → hard rule: “should” became “must” (or vice versa)
Closing thought
Policy change is not mysterious—it’s procedural. When you capture the who/what/when/why at each stage and keep the raw text alongside the normalized summary, you turn “because we said so” into a traceable narrative. That’s how you explain a denial, forecast a shift, and defend a decision—all without relying on any particular platform or vendor.