Introduction
Healthcare Team Dynamics: The Pharmacist’s Position
Pharmacists occupy a unique position in healthcare, interfacing directly with patients, providers, and the broader medical community. Their expertise in medication management makes them indispensable for ensuring safe and effective therapy regimens. As the medication experts, pharmacists are well-equipped to facilitate communication among healthcare professionals, patients, and other stakeholders.
Goal: Maximizing Patient Care Through Collaboration
The primary objective of collaborative efforts is to optimize patient outcomes. By working closely with adjacent stakeholders, pharmacists can contribute to a more cohesive healthcare delivery model. This collaborative approach leads to improved medication adherence, reduced errors, and enhanced overall patient satisfaction.
I. Identifying Stakeholders
Internal Teams: Physicians, Nurses, and Administrators
- Physicians: Collaborate on prescribing practices and medication therapy management.
- Nurses: Coordinate on patient education and administration of medications.
- Administrators: Align on policy implementation, formulary decisions, and resource allocation.
External Partners
- Suppliers: Ensure a consistent supply of high-quality medications.
- Insurers: Work with health plans to understand coverage and reimbursement policies.
- Community Organizations: Partner on public health initiatives and patient outreach programs.
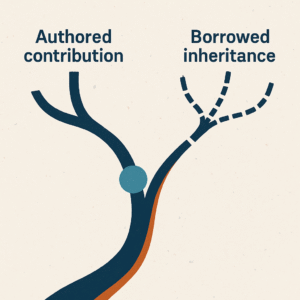
Pharma Representatives and PBM Experts
Health plan clinicians often interact with pharmaceutical company representatives who advocate for their products. These interactions are crucial for:
- Understanding New Therapies: Gaining insights into the latest medications and their clinical benefits.
- Negotiating Contracts: PBM experts assist in securing favorable terms, ensuring compliance, and developing programs that benefit both the plan and its members.
II. Communication Strategies
Effective Dialogue: Clear and Concise Information Sharing
- Active Listening: Understand the perspectives and needs of other stakeholders.
- Transparent Communication: Share information openly to build trust and facilitate decision-making.
- Tailored Messaging: Present information in a way that is relevant to each stakeholder’s interests and expertise.
Interdisciplinary Meetings: Regular Collaboration Forums
- Scheduled Meetings: Establish routine check-ins with internal and external teams.
- Joint Committees: Participate in formulary committees and medication safety teams.
- Virtual Collaboration Tools: Utilize technology to facilitate communication across different locations.
III. Collaborative Initiatives
Medication Reconciliation: Joint Efforts to Prevent Errors
- Process Standardization: Develop protocols with input from all stakeholders to ensure consistency.
- Data Sharing: Use shared electronic health records (EHRs) to keep all parties informed.
- Patient Involvement: Educate patients to be active participants in their medication management.
Health Education Programs: Partnering on Patient Outreach
- Community Workshops: Collaborate with community organizations to host educational events.
- Wellness Campaigns: Work with insurers and PBMs to promote preventive care and medication adherence.
- Digital Platforms: Use social media and apps to reach a broader audience.
IV. Overcoming Barriers
Cultural Differences: Bridging Gaps Between Professions
- Interprofessional Education: Engage in training that fosters understanding of different roles.
- Team-Building Activities: Participate in exercises that strengthen relationships among team members.
- Respect and Empathy: Acknowledge the expertise and contributions of all stakeholders.
Resource Constraints: Optimizing Limited Assets
- Efficient Workflows: Implement systems that reduce redundancy and streamline processes.
- Shared Resources: Pool resources with external partners for mutual benefit.
- Advocacy: Lobby for policies that provide adequate funding and support for collaborative initiatives.
V. Measuring Success
Outcome Metrics: Assessing the Impact on Patient Care
- Clinical Outcomes: Monitor improvements in patient health indicators.
- Medication Adherence Rates: Track compliance to prescribed regimens.
- Error Reduction: Evaluate the decrease in medication errors and adverse events.
Feedback Loops: Continuous Improvement Through Evaluations
- Stakeholder Surveys: Gather input from team members and patients.
- Performance Reviews: Regularly assess collaborative efforts and identify areas for enhancement.
- Data Analysis: Use analytics to inform decision-making and demonstrate value.
Conclusion
Collective Responsibility: Enhancing Healthcare Through Teamwork
Collaboration among pharmacists, healthcare professionals, and adjacent stakeholders is essential for delivering high-quality patient care. By recognizing and embracing their interconnected roles, these professionals can create a more efficient, effective, and patient-centered healthcare system.
Pharmacist Leadership: Taking Initiative in Collaborative Efforts
Pharmacists are uniquely positioned to lead collaborative initiatives due to their comprehensive understanding of medication management and patient care. By proactively engaging with internal teams, external partners, pharma representatives, and PBM experts, pharmacists can drive meaningful change and expand their impact within the healthcare landscape.