Introduction
Pharmacy & Therapeutics (P&T) committees have long been the cornerstone of drug coverage decisions, governing what medications are included on formularies and under what criteria. Historically, these committees comprised a select few clinical and administrative experts. While this centralized model helped ensure consistency, it often lacked transparency and provided limited opportunities for real-time updates or broader stakeholder input. As prescription drug costs and complexities continue to rise, many in the industry are asking: Is there a better way to decide what medications patients can access?
Drivers of Change
Several forces are converging to reshape how P&T decisions are made. First, a public push for transparency has revealed hidden fees and spread pricing, driving demand for more open, data-driven negotiations. Second, AI-driven analytics enable quicker and more accurate assessments of clinical outcomes, cost-effectiveness, and patient-specific needs and coverage conditions. Finally, employers and health plan users themselves are demanding more personalized, value-oriented deals—especially in a climate of rising specialty drug costs. These factors set the stage for a transformative shift from the traditional P&T model toward a more dynamic, inclusive system.
P&TaaS and the Future Exchange
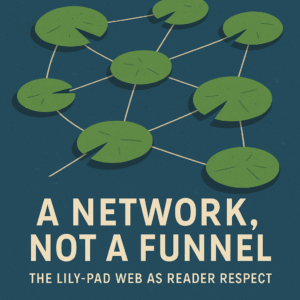
One emerging concept is “P&T-as-a-Service” (P&TaaS)—a platform-driven approach that merges the best of formal clinical review with a dynamic marketplace for negotiations. Rather than one group making decisions behind closed doors, an exchange-like forum could invite drug manufacturers, payers, and even patient advocacy groups to propose and evaluate different or exhaustive coverage scenarios. Clinical experts would still guide evidence-based decisions, but market-driven mechanisms—like auctions, bids, or tiered offers—could expedite the process and keep drug coverage rules updated in near-real time.
Operational Blueprint
Imagine a real-time data feed pulling in new clinical studies, patient outcomes, and cost metrics. This feed updates the exchange forum, triggering automated alerts when a drug becomes more cost-effective or a novel therapy gains FDA approval and alters the coverage landscape. Compliance checks and automated guardrails ensure the forum adheres to state and federal regulations, including HIPAA and FDA promotional guidelines. Manufacturers post bids or rebate offerings directly to the platform, visible to payers who can sort options by budget impact and clinical value. Meanwhile, a committee oversight team—composed of pharmacists, clinicians, and perhaps employer representatives—validates critical decisions, preserving the clinical integrity of P&T rulings.
Advantages and Potential Obstacles
A key advantage of this exchange forum is faster updates. Rather than waiting months for the next P&T meeting, coverage decisions could be made (or revised) within days. Additionally, a broader group of stakeholders—including patient representatives and smaller self-insured employers—gains visibility into negotiations, potentially driving more equitable and cost-effective drug coverage. Still, challenges remain. Such a system demands a robust governance structure, sophisticated data integration, and strict privacy controls. Not all entities will readily adapt to sharing pricing or clinical data so transparently.
Conclusion
In a landscape where drug costs continue to rise and tech innovation is outpacing traditional healthcare decision-making models, an exchange-like platform offers a new horizon for P&T. It combines the rigor of clinical oversight with the real-time benefits of marketplace dynamics. By embracing transparency and stakeholder engagement, this next-generation approach has the potential to democratize and modernize drug coverage decisions, ultimately delivering more value to plans, payers, and—most importantly—patients.
FAQ
1. What is a traditional P&T committee?
A Pharmacy & Therapeutics committee is a group of healthcare professionals who decide which medications are covered on a formulary. Historically, these committees have operated with limited stakeholder input.
2. What does “P&T-as-a-Service” mean?
P&TaaS refers to an outsourced or platform-based approach where clinical reviews and market negotiations happen in a more transparent, dynamic forum—akin to an online marketplace.
3. How does an exchange forum improve drug coverage decisions?
By inviting manufacturers, payers, and patient advocacy groups to participate, an exchange forum fosters transparent negotiations, data-driven decisions, and faster updates when clinical or cost factors change.
4. Are there compliance concerns with a more open system?
Yes. Privacy laws like HIPAA and state-level regulations must be upheld. Automated compliance checks and strict governance structures are crucial for maintaining patient confidentiality and data security.
5. Who benefits from a next-generation P&T model?
Employers, health plans, and patients all stand to gain. Employers and payers can reduce costs through competitive bidding and dynamic formulary updates, while patients enjoy improved access to the most effective, affordable medications.