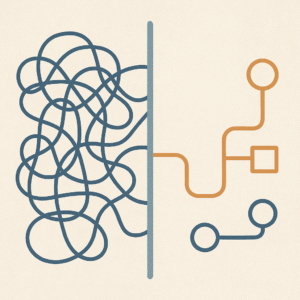
Introduction: Why Enumerated Node-Based Coverage?
For years, pharmacy benefit managers (PBMs) have acted as gatekeepers for drug coverage, often obscuring true costs and clinical rules behind opaque formularies. While these intermediaries once promised efficiency, many stakeholders—manufacturers, payers, and patient advocacy groups—are now calling for a more transparent and flexible model. Enumerated node-based coverage presents a radical alternative: a network of coverage “nodes” that expose real-time price and clinical rules, forcing manufacturers to consider an exhaustive approach to how their products will be priced in a competitive market. The result? More flexible negotiations, clearer costs, and greater freedom to tailor benefits for specific populations.
Defining the Coverage Node
A coverage node is a singular point in the pharmacy benefit universe, reflecting price, clinical rules, and coverage conditions for a specific dose or drug. Instead of a single PBM imposing one-size-fits-all coverage restrictions, each node offers its own coverage criteria combinations at market-based rates. The assumption is that every node will ultimately provide coverage of some kind; however, the parameters within a drug’s criteria library will drive the negotiations to achieve market rate.
This decentralized network redefines the manufacturer–payer/PBM interface by requiring manufacturers to agree to a price and criteria coverage terms for each node. Manufacturers can no longer rely on a single rebate or discount strategy; they have to consider many potential coverage scenarios. If a particular node’s approach fails to deliver clinical value, payers can simply turn it off, thus incentivizing better alignment with cost-effectiveness and patient outcomes. If another competitor is pricing more aggressively for a particular criteria combination, then prices can be driven lower for the same clinical outcome.
Shared Secrets and Open Information
One core element of enumerated node-based coverage is the shared secrets model. The latest price or coverage criteria for a given node becomes publicly available to all participants. For example, if the makers of Crestor lower the rate for individuals with LDL values above 200, the makers of Lipitor can instantly react and adjust its rate as well. Rather than operating behind closed doors, manufacturers compete in a transparent, open-information market. This real-time “price discovery” pressures costs and helps align coverage with valuable care.
Destroying the Concept of Co-pays
Traditionally, patients face copays or coinsurance that can obscure true drug costs, especially with numerous benefit phases. Under enumerated node-based coverage, there is only one true cost—the real net price for each medication claim or fill. Plan sponsors will no longer need to hide behind labyrinthine tiers or variable out-of-pocket fees. Instead, benefit design focuses on ensuring all net costs are known or at least easier to predict and manage. Risk managers shouldn’t conduct business exploitatively based on information disparities. By eliminating copays, stakeholders can streamline cost structures, making it clearer when a particular medication truly provides value.
How It Works: Turning Nodes On (or Off)
-
- Coverage Enumeration: Each node for any managed drug is enumerated, which will capture coverage and price details for a specific drug (e.g., guideline recommended prior authorization rules, population eligibility, and net cost).
-
- Market Rate Updates: Whenever a manufacturer lowers (or raises) its rate, that new price is published immediately. Competing manufacturers can respond immediately as well, driving down overall costs.
-
- Node Evaluation: If a node fails to meet clinical expectations or deliver cost-effectiveness, payers can disable that node. This ensures only high-performing options remain.
-
- Open Marketplace: Providers or plan sponsors “shop around” to evaluate which node mix delivers the best combination of cost, outcome, and patient-centric rules.
-
- Provider Request Opt-ins: Similar to DAW codes, a provider engaging with the coverage enumeration network can opt to allow the network to decide the best coverage node based on the patient’s condition. The best option will be transparently selected if there are several safe and effective alternatives.
Tailored Solutions for Diverse Populations
The granular, competitive nature of enumerated nodes allows for highly targeted coverage solutions. For instance:
-
- Pediatrics: A network of nodes tailored for pediatric dosages can outline best practices for various unique disease states, from drug safety profiles to price points parents can afford.
-
- Rare Diseases: Nodes may offer valuable data for orphan drugs, gathering enough critical mass to offer feedback on the RWE populations that the drug is reaching, and the coverage conditions that were met at time of dispensing.
-
- General Chronic Conditions: For high-prevalence conditions such as diabetes or multiple sclerosis, various nodes compete on both price and clinical guidelines, creating a race to the top in verifiable evidence superiority.
Conclusion: A Paradigm Shift in Pharmacy Benefits
Enumerated node-based coverage stands poised to replace conventional PBM strategies with a transparent, flexible, and dynamic system. By destroying copays, embracing real net cost disclosures, and allowing stakeholders to exhaustively negotiate and potentially switch off underperforming nodes, payers regain control over nuanced coverage decisions. Meanwhile, manufacturers face increased pressure to deliver competitive pricing and robust clinical outcomes for distinct patient populations.
Though operational challenges remain—such as building the technical infrastructure for real-time updates—this model aligns well with a future where multiple stakeholders, from employers to advocacy groups, demand open information. By decentralizing coverage details and requiring exhaustive manufacturer participation, enumerated node-based coverage can shape a more equitable and cost-effective drug ecosystem—one that more effectively places access and clinical value at the forefront.